Waldorf News
The Myopia Boom Short-sightedness is reaching epidemic proportions. Some scientists think they have found a reason why.

The southern city of Guangzhou has long held the largest eye hospital in China. But about five years ago, it became clear that the Zhongshan Ophthalmic Center needed to expand.
More and more children were arriving with the blurry distance vision caused by myopia, and with so many needing eye tests and glasses, the hospital was bursting at the seams. So the centre began adding new testing rooms — and to make space, it relocated some of its doctors and researchers to a local shopping mall. Now during the summer and winter school holidays, when most diagnoses are made, “thousands and thousands of children” pour in every day, says ophthalmologist Nathan Congdon, who was one of those uprooted. “You literally can’t walk through the halls because of all the children.”
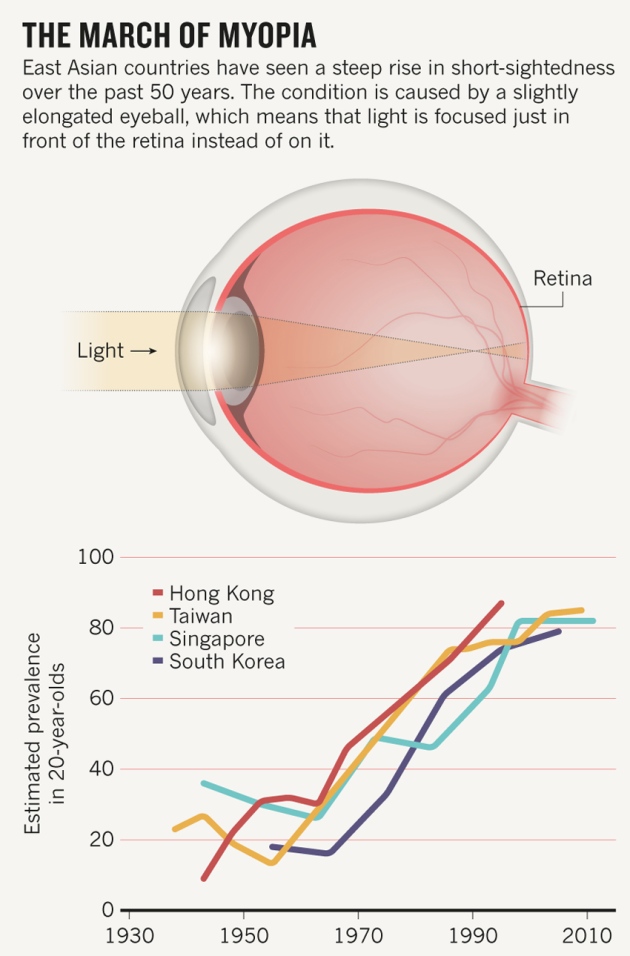
East Asia has been gripped by an unprecedented rise in myopia, also known as short-sightedness. Sixty years ago, 10–20% of the Chinese population was short-sighted. Today, up to 90% of teenagers and young adults are. In Seoul, a whopping 96.5% of 19-year-old men are short-sighted.

Other parts of the world have also seen a dramatic increase in the condition, which now affects around half of young adults in the United States and Europe — double the prevalence of half a century ago. By some estimates, one-third of the world’s population — 2.5 billion people — could be affected by short-sightedness by the end of this decade. “We are going down the path of having a myopia epidemic,” says Padmaja Sankaridurg, head of the myopia programme at the Brien Holden Vision Institute in Sydney, Australia.
The condition is more than an inconvenience. Glasses, contact lenses and surgery can help to correct it, but they do not address the underlying defect: a slightly elongated eyeball, which means that the lens focuses light from far objects slightly in front of the retina, rather than directly on it. In severe cases, the deformation stretches and thins the inner parts of the eye, which increases the risk of retinal detachment, cataracts, glaucoma and even blindness. Because the eye grows throughout childhood, myopia generally develops in school-age children and adolescents. About one-fifth of university-aged people in East Asia now have this extreme form of myopia, and half of them are expected to develop irreversible vision loss.
This threat has prompted a rise in research to try to understand the causes of the disorder — and scientists are beginning to find answers. They are challenging old ideas that myopia is the domain of the bookish child and are instead coalescing around a new notion: that spending too long indoors is placing children at risk. “We’re really trying to give this message now that children need to spend more time outside,” says Kathryn Rose, head of orthoptics at the University of Technology, Sydney.
Vision quest
For many years, the scientific consensus held that myopia was largely down to genes. Studies in the 1960s showed that the condition was more common among genetically identical twins than non-identical ones, suggesting that susceptibility is strongly influenced by DNA. Gene-finding efforts have now linked more than 100 regions of the genome to short-sightedness.

Singapore National Myopia Programme/Health Promotion Board. A Singapore poster encourages children to spend time outside to prevent myopia.
But it was obvious that genes could not be the whole story. One of the clearest signs came from a 1969 study of Inuit people on the northern tip of Alaska whose lifestyle was changing. Of adults who had grown up in isolated communities, only 2 of 131 had myopic eyes. But more than half of their children and grandchildren had the condition. Genetic changes happen too slowly to explain this rapid change — or the soaring rates in myopia that have since been documented all over the world (see ‘The march of myopia’). “There must be an environmental effect that has caused the generational difference,” says Seang Mei Saw, who studies the epidemiology and genetics of myopia at the National University of Singapore.
There was one obvious culprit: book work. That idea had arisen more than 400 years ago, when the German astronomer and optics expert Johannes Kepler blamed his own short-sightedness on all his study. The idea took root; by the nineteenth century, some leading ophthalmologists were recommending that pupils use headrests to prevent them from poring too closely over their books.
The modern rise in myopia mirrored a trend for children in many countries to spend more time engaged in reading, studying or — more recently — glued to computer and smartphone screens. This is particularly the case in East Asian countries, where the high value placed on educational performance is driving children to spend longer in school and on their studies. A report last year from the Organisation for Economic Co-operation and Development showed that the average 15-year-old in Shanghai now spends 14 hours per week on homework, compared with 5 hours in the United Kingdom and 6 hours in the United States.
Researchers have consistently documented a strong association between measures of education and the prevalence of myopia. In the 1990s, for example, they found that teenage boys in Israel who attended schools known as Yeshivas (where they spent their days studying religious texts) had much higher rates of myopia than did students who spent less time at their books. On a biological level, it seemed plausible that sustained close work could alter growth of the eyeball as it tries to accommodate the incoming light and focus close-up images squarely on the retina.
Attractive though the idea was, it did not hold up. In the early 2000s, when researchers started to look at specific behaviours, such as books read per week or hours spent reading or using a computer, none seemed to be a major contributor to myopia risk. But another factor did. In 2007, Donald Mutti and his colleagues at the Ohio State University College of Optometry in Columbus reported the results of a study that tracked more than 500 eight- and nine-year-olds in California who started out with healthy vision. The team examined how the children spent their days, and “sort of as an afterthought at the time, we asked about sports and outdoorsy stuff”, says Mutti.
It was a good thing they did. After five years, one in five of the children had developed myopia, and the only environmental factor that was strongly associated with risk was time spent outdoors. “We thought it was an odd finding,” recalls Mutti, “but it just kept coming up as we did the analyses.” A year later, Rose and her colleagues arrived at much the same conclusion in Australia. After studying more than 4,000 children at Sydney primary and secondary schools for three years, they found that children who spent less time outside were at greater risk of developing myopia.
Source: Ian Morgan, Australian Natl Univ.
Rose’s team tried to eliminate any other explanations for this link — for example, that children outdoors were engaged in more physical activity and that this was having the beneficial effect. But time engaged in indoor sports had no such protective association; and time outdoors did, whether children had played sports, attended picnics or simply read on the beach. And children who spent more time outside were not necessarily spending less time with books, screens and close work. “We had these children who were doing both activities at very high levels and they didn’t become myopic,” says Rose. Close work might still have some effect, but what seemed to matter most was the eye’s exposure to bright light.
See the light
Some researchers think that the data to support the link need to be more robust. Most epidemiological studies have estimated children’s time outdoors from questionnaires — but Christine Wildsoet, an optometrist at the University of California, Berkeley, says that such data should be treated with caution. In a small, pilot study of wearable light sensors, she found that people’s estimates often do not match up with their actual exposure. And Ian Flitcroft, a myopia specialist at Children’s University Hospital in Dublin, questions whether light is the key protective factor of being outdoors. He says that the greater viewing distances outside could affect myopia progression, too. “Light is not the only factor, and making it the explanation is a gross over-simplification of a complex process,” he says.
Yet animal experiments support the idea that light is protective. Researchers first demonstrated this in chicks, a common lab model for studying vision. By fitting chicks with goggles that alter the resolution and contrast of incoming images, it is possible to induce the development of myopia while raising the birds under controlled conditions in which only light intensity is changed. In 2009, Regan Ashby, Arne Ohlendorf and Frank Schaeffel from the University of Tübingen’s Institute for Ophthalmic Research in Germany showed that high illumination levels — comparable to those encountered outside — slowed the development of experimentally induced myopia in chicks by about 60% compared with normal indoor lighting conditions. Researchers elsewhere have found similar protective effects in tree shrews and rhesus monkeys.
But what scientists really needed was a mechanism: something to explain how bright light could prevent myopia. The leading hypothesis is that light stimulates the release of dopamine in the retina, and this neurotransmitter in turn blocks the elongation of the eye during development. The best evidence for the ‘light–dopamine’ hypothesis comes — again — from chicks. In 2010, Ashby and Schaeffel showed that injecting a dopamine-inhibiting drug called spiperone into chicks’ eyes could abolish the protective effect of bright light.
Retinal dopamine is normally produced on a diurnal cycle — ramping up during the day — and it tells the eye to switch from rod-based, nighttime vision to cone-based, daytime vision. Researchers now suspect that under dim (typically indoor) lighting, the cycle is disrupted, with consequences for eye growth. “If our system does not get a strong enough diurnal rhythm, things go out of control,” says Ashby, who is now at the University of Canberra. “The system starts to get a bit noisy and noisy means that it just grows in its own irregular fashion.”
Time out
Based on epidemiological studies, Ian Morgan, a myopia researcher at the Australian National University in Canberra, estimates that children need to spend around three hours per day under light levels of at least 10,000 lux to be protected against myopia. This is about the level experienced by someone under a shady tree, wearing sunglasses, on a bright summer day. (An overcast day can provide less than 10,000 lux and a well-lit office or classroom is usually no more than 500 lux.) Three or more hours of daily outdoor time is already the norm for children in Morgan’s native Australia, where only around 30% of 17-year-olds are myopic. But in many parts of the world — including the United States, Europe and East Asia — children are often outside for only one or two hours.
“Sort of as an afterthought, we asked about sports and outdoorsy stuff.”
In 2009, Morgan set out to test whether boosting outdoor time would help to protect the eyesight of Chinese children. He and a team from the Zhongshan Ophthalmic Center (where Morgan also works) launched a three-year trial in which they added a 40-minute outdoor class to the end of the school day for a group of six- and seven-year-olds at six randomly selected schools in Guangzhou; children at six other schools had no change in schedule and served as controls. Of the 900-plus children who attended the outside class, 30% developed myopia by age nine or ten compared with 40% of those at the control schools. The study is being prepared for publication.
A stronger effect was found at a school in southern Taiwan, where teachers were asked to send children outside for all 80 minutes of their daily break time instead of giving them the choice to stay inside. After one year, doctors had diagnosed myopia in 8% of the children, compared with 18% at a nearby school12.
Morgan is buoyed by the preliminary findings, but thinks that he can do even better. “We’ve got proof of principle that increasing the amount of time children spend outside actually works,” he says. “The question then is how do we make this work in practice at a level that would have a significant impact?” He recognizes that many schools do not have the flexibility to add time outdoors. So last year, in collaboration with Congdon, he began piloting the idea of teaching kids in a classroom made of glass to let in more natural light. “This glass classroom idea is quite applicable for whole swathes of China,” Congdon says.
Rose points out that additional outdoor time “has to be mandated through the schools, because getting parents to voluntarily do this is extremely difficult”. Saw and her colleagues learned this when they trialled a 9-month programme to teach parents in Singapore about the importance of outdoor time in order to prevent myopia. They provided step-counters, organized outdoor weekend activities for families and even offered cash prizes for cooperation. But by the end of the trial, the time spent outdoors was not statistically different from that for a control group with no such campaign.
In some places, children cannot get any more outdoor light: there are too few hours of daylight, the sun is too fierce, or the cold too intense. Animal research has suggested that powerful indoor lights could do the trick instead: light boxes currently sold to treat seasonal affective disorder, for example, can deliver up to 10,000 lux illumination, but their effects on myopia have not been tested extensively in humans.
Meanwhile, researchers have been working on ways to prevent myopia from worsening. Sankaridurg and her colleagues have developed special glasses and contact lenses that can alter eye growth by focusing light from distant images across the entire field of view, rather than just at the centre, as standard lenses do. Other research groups have shown that nightly eye drops with a neurotransmitter-blocking drug called atropine can also help to control myopia progression, although the mechanism remains unclear. “We want to take a holistic approach” to tackling myopia, Sankaridurg says.
But eye drops and light boxes do not have quite the appeal of sending children outside to play, which has plenty of other benefits besides those for the eyes. “It probably also increases physical activity, which decreases likelihood of obesity and enhances mood,” Rose says. “I can only see it as a win — and it’s free.”
More than a century ago, Henry Edward Juler, a renowned British eye surgeon, offered similar advice. In 1904, he wrote in A Handbook of Ophthalmic Science and Practice that when “the myopia had become stationary, change of air — a sea voyage if possible — should be prescribed”. As Wildsoet points out: “We’ve taken a hundred years to go back to what people were intuitively thinking was the case.”
This article originally appeared in “Nature.” To view the article at source at nature.com, just click here.
 Jamie York Books, Resources, Workshops
Jamie York Books, Resources, Workshops Roadmap to Literacy Books & Courses
Roadmap to Literacy Books & Courses Caring for All Stages of Life
Caring for All Stages of Life Waldorf Training in Australia
Waldorf Training in Australia Space speaks. Its language is movement.
Space speaks. Its language is movement. Transforming Voices Worldwide
Transforming Voices Worldwide
 Quality Education in the Heartland
Quality Education in the Heartland ~ Ensoul Your World With Color ~
~ Ensoul Your World With Color ~ Bay Area Teacher Training
Bay Area Teacher Training Everything a Teacher Needs
Everything a Teacher Needs The Journey is Everything
The Journey is Everything Middle School Science With Roberto Trostli
Middle School Science With Roberto Trostli Bringing Love to Learning for a Lifetime
Bringing Love to Learning for a Lifetime Association for a Healing Education
Association for a Healing Education Flexible preparation for your new grade
Flexible preparation for your new grade Train to Teach in Seattle
Train to Teach in Seattle Immersive Academics and Arts
Immersive Academics and Arts Great books for Waldorf Teachers & Families
Great books for Waldorf Teachers & Families Apply Today: New Cohort Starts Nov. 2025
Apply Today: New Cohort Starts Nov. 2025 Full-Time Teacher Education
Full-Time Teacher Education Summer Programs - Culminating Class Trips
Summer Programs - Culminating Class Trips Waldorf-inspired Homeschool Curriculum
Waldorf-inspired Homeschool Curriculum RSS Feeds
RSS Feeds